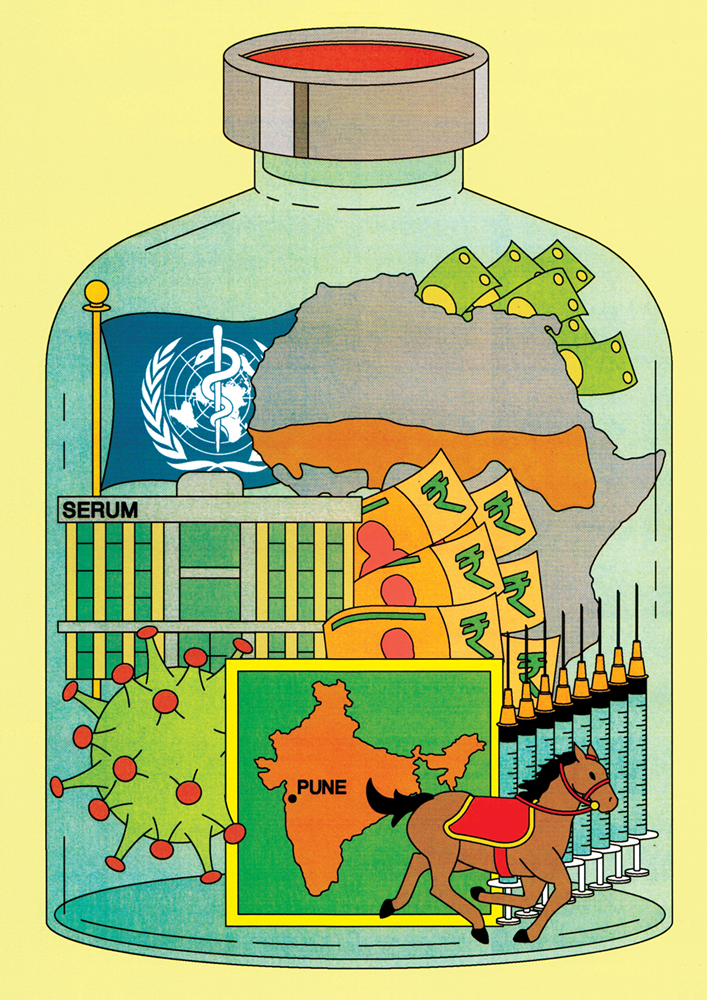
Before starting what would become the world’s largest manufacturer of vaccines, Cyrus Poonawalla was destined to become a horse breeder. Born in 1941 into a Pune based business family, Poonawalla grew up around India’s horseracing circuit. When Poonawalla was five, his father, Soli, founded the Poonawalla Stud Farm, which became one of the premier breeding facilities in Asia. But by the time Cyrus reached his 20s, the future of the family horse farm looked uncertain. The chief minister of the erstwhile western state of Bombay had recently banned horse races.
Poonawalla tried his hand at other ventures — he prototyped a sports car modeled after a Jaguar — before a chance conversation with a veterinarian at the horse farm led him to a new idea: antitoxins. Like vaccines, antitoxins protect people against pathogens — for example, the tetanus causing Clostridium tetani. But, unlike vaccines, which coax the body into making its own antibodies and other immune cells, antitoxins contain readymade antibodies.
In the 1960s, the most efficient way to manufacture antitoxins was through horses. Horses are immunized with gradually increasing doses of a specific toxin. Over time, they develop high levels of antibodies, which are extracted and purified from their blood serum. And in India, antitoxins were in short supply.
Cyrus Poonawalla had horses. So, in 1966, he invested Rs 99,000 ($12,000) to found an anti-toxin manufacturing company, which he called the Serum Institute of India. Its first product was a tetanus antitoxin. For the technology and know how, Poonawalla hired and consulted employees from India’s government manufacturers, then the major producers of both antitoxins and vaccines throughout the country. Within a few years, Serum diversified into vaccines. By 1974, the firm produced both a tetanus vaccine and a combined vaccine against diphtheria, tetanus and whooping cough, or DTP — both staples of childhood immunization programs.
Fast forward 50 years: By early 2024, Serum had manufactured and shipped more than two billion COVID-19 vaccines to over 170 countries, more than any other supplier. According to Serum, some 65% of all children are estimated to have received at least one vaccine manufactured by Serum. From its humble origins at a racetrack — and despite an over 100 year headstart over manufacturers like Pfizer — Serum has become the largest, and generally most affordable, supplier of vaccines around the world.
Immunizing India
The global vaccine industry can be divided into two parts. Manufacturers in high income countries — British GlaxoSmithKline, American Merck and Pfizer, and French Sanofi — represent some 70% of the worldwide market share for vaccines by value. These companies have huge budgets for R&D, and are generally the first to release best in class products. But their prices are high and their volumes are often low. As a result, most of what they manufacture remains out of reach, both logistically and economically, for much of the developing world.
Alternatives to these “Big Four” manufacturers started to crop up in the second half of the 20th century, due to the efforts of global health organizations as well as developing country ambitions to become self sufficient in vaccine production. Vaccine manufacturers arose in places like China, India, and Indonesia, making more affordable products for largely domestic consumers. These manufacturers in low and middle income countries are celebrated heroes in public health circles — underdogs who overcame R&D budget constraints to bring vaccines to some of the world’s poorest countries.
But few LMIC manufacturers are as celebrated as Serum.
The late sixties proved a good time for a private manufacturer to enter the Indian market. Government manufacturers, hobbled by underfunding and bureaucratic deadlock, were beginning to lose their edge, while Indian demand for vaccines was rising. In 1974, the World Health Organisation called upon member states to introduce the Expanded Program on Immunization (EPI), a drive to immunize all children against major childhood diseases. India developed its own EPI in 1978, focused on four of the recommended vaccinations: BCG (for tuberculosis), DPT, an oral polio vaccine, and a typhoid vaccine.
A key recommended vaccine on the WHO’s EPI, but not on India’s, was measles. One major reason is that the perceived disease burden of measles in India was low. India had minimal national surveillance, and health officials assumed it was not a common problem. But India also lacked domestic manufacturing technology for a measles vaccine and had a limited cold chain infrastructure to support its delivery. BCG, DPT, and typhoid were all bacterial vaccines which Indian vaccine manufacturers — like Serum — could manufacture domestically. The vaccines for oral polio and measles, both viral diseases, were more recent technological advancements, but oral polio vaccines could at least be imported cheaply. Measles vaccines could not.
Then, a series of studies in the early 1980s showed that the measles burden in India was far larger than previously appreciated. In 1985, India upgraded its EPI into the Universal Immunization Programme, which this time included measles. It also set two ambitious goals: to reach 85% of all children by 1990 and to achieve self sufficiency in vaccine production.
Serum, as a private company that could make decisions quicker than government manufacturers, was well positioned to fill this market gap. In the mid 1980s, it licensed the technology for a measles vaccine from a Yugoslavian government institution, the Institute of Immunology in Zagreb. At the time, Zagreb had a strong vaccine research program. It had developed its own measles vaccine, which had become as widely used across the world as the original measles vaccine strain developed in the US. Around the same time, Serum received a grant of around $400,000 from USAID to buy manufacturing equipment for the measles vaccine.
With the technology and funding in hand, Serum got its vaccine licensed by Indian regulators in 1989. Now it had a globally accepted technology, made in a world class facility, which enabled the company to make another strategic decision that would set it apart from other Indian manufacturers: Serum was going to expand beyond the Indian markets and sell to the United Nations.
The shift to international markets
Throughout the decade, more LMICs launched their own EPIs. This led to UN agencies procuring vaccines in large numbers on their behalf. Cyrus Poonawalla was quick to seize on this new market opportunity, frustrated as he was with his primary client: the Indian government. Poonawalla claims that the government was often chronically delayed in making payments to Serum in its early days, putting the company under financial stress.
A second development in the 1980s made the global child immunization market easier to access, according to Raman Rao, chief executive officer of the Singapore based vaccine research company Hilleman labs. The WHO Prequalification Program, launched in 1987, certified to UN buyers that a given vaccine met international standards for quality, safety, and efficacy. Before prequalification, manufacturers who wanted to sell their products internationally also had to contend with varying regulatory standards across countries. The US Food & Drug Administration, for example, was among the best resourced and most stringent regulators in the world, while the Drug Controller General of India, was a fledgling agency, still learning how to regulate the latest technological advancements.
The WHO prequalification program brought all UN suppliers to the same level. Prequalification was a globally respected stamp of quality, unlike approval from the Indian vaccine regulator. Poonawalla and his team pursued this opportunity aggressively. They applied to the WHO for prequalification for their measles vaccine, which they believed was their best candidate. “The choice of the measles vaccine as Serum’s first WHO PQ candidate was a tactical decision. It was a lower risk product — technically established, already licensed in India, and developed using internationally recognized strains acquired from Zagreb,” a Serum spokesperson said. Serum’s measles vaccine was prequalified in 1993, among the first vaccines from any LMIC manufacturer to receive this recognition.
Other Indian contemporaries of Serum were slower to pursue the WHO prequalification opportunity: Biological E, founded in 1953, received its first prequalification only in 2009. Meanwhile, Serum moved fast: By 2000, it had over half a dozen prequalified vaccines. Today, it has more than 20, making it the manufacturer with the largest number of prequalified vaccines in the world, and among the largest suppliers to UN agencies.
In retrospect, Serum’s move to the UN markets was a shrewd one. It gave the company a reputation for quality, at a time when Indian manufacturers didn’t have it. Compared to the Indian government, UN agencies paid promptly for childhood vaccines. They also paid more. Most importantly, Serum’s international presence gave it an advantage in pursuing new philanthropy funded opportunities that would emerge in the coming years.
Many of these opportunities came through the Bill & Melinda Gates Foundation. A key goal of the Gates Foundation was to improve access to quality vaccines in LMICs, both by incentivizing more manufacturers to make vaccines through R&D grants, and by incentivizing governments to buy them through institutions like GAVI, a pooled procurement program.
Serum benefited from both: Several of the vaccines in its portfolio today were developed with help from Gates Foundation, and 14 of them are sold to GAVI.
The first vaccine that Serum developed with funding from Gates was a jab against meningitis. Like most of Serum’s products, the meningitis vaccine was, strictly speaking, a “me too” or second generation vaccine — a cheaper version of a vaccine that was already licensed in the global north. But Serum’s collaborators on the project say the phrase “me too” doesn’t fully capture the value of the meningitis vaccine and Serum’s subsequent products. While producing a second generation vaccine is less technically complex than developing a first in class product, it doesn’t mean the vaccine has no new technology. And sometimes, the new technologies in second generation vaccines dramatically expand their public health impact.
This is what Serum and its partners did with MenAfriVac.
MenAfriVac: more than a “me too” jab
The African Meningitis Belt is a strip of land spanning over two dozen countries, from Senegal to Ethiopia. The area is subject to yearly Harmattan winds, which bring dust storms that irritate mucus membranes and increase susceptibility to the disease. The rain storms that mark the end of the season have been described as the best vaccine for meningitis. Historically, the region experienced periodic outbreaks in time with the winds, with incidence as high as one in 100 during severe years.
Meningitis can be caused by many different bacteria, but the most common culprit in African outbreaks at that time was Neisseria meningitidis, serotype A. Fatality rates from this serotype can be as high as 15% — children are particularly vulnerable, and the population in most African countries skews young. A similar proportion of survivors experience permanent disabilities, including hearing or vision loss.
Meningitis vaccines have been around since the early 1970s, when French researchers produced the first polysaccharide shots. However, these only conferred short term protection and could thus only be used reactively in response to active outbreaks. They did little to prevent future epidemics. And they were ineffective in children.
A breakthrough came in the 1990s with the development of conjugate vaccines. Polysaccharide vaccines contain polysaccharides, or sugar molecules, found on the surface of the target bacteria. In the body, they stimulate B cells to produce antibodies. What they can’t do is stimulate T cells, which form the basis of the body’s immune memory. In contrast, a meningococcal conjugate vaccine works by chemically linking the bacterium’s capsular polysaccharide to a carrier protein—usually tetanus or diphtheria toxoid. The protein tag recruits helper T cells, which in turn generate long lived memory B cells and high quality IgG antibodies. The result is long term protection.
The first conjugate vaccine, designed for N. meningitidis serotype C, worked brilliantly in the UK, where it reduced fatalities from the hundreds to less than 10 in 2001. A conjugate shot developed by French manufacturer Sanofi for serotype A came just a few years later. However, it was expensive — at between $50 to 100 per dose, the price was far beyond what any African country could afford. It also required cold chain distribution, making it unsuitable for deployment across the meningitis belt.
To solve this sticky problem, in 2001, the WHO formed a partnership with PATH, a global health nonprofit, called the Meningitis Vaccine Project. It would act like a virtual company pooling the resources of multiple organisations, a model sometimes called a Product Development Partnership. Initially, MVP invited established western manufacturers to join the partnership. To entice them, MVP, with funding from the Gates Foundation, offered to help the manufacturers with upfront costs to develop and test vaccine candidates. With those costs covered, manufacturers could still turn a profit selling the vaccine for under 50 cents — the maximum price African governments said they could afford.
No western manufacturers bit. The vaccines in their pipelines, aimed at wealthier markets, promised far greater profits. In other words, even though these manufacturers could profit from the meningitis A vaccine, their opportunity cost was too high.
For the first time, MVP looked to manufacturers in the developing world, even though many in global public health circles believed they were too inexperienced for a project of such complexity. Marc LaForce, a meningitis vaccine specialist who headed the project, said in an interview that his team shortlisted five of the most promising candidates, including Brazilian, Cuban and Indian firms. But only one of those companies had already made several WHO prequalified vaccines: Serum. “It was easily the winner, the company that was the farthest along, the safest investment,” LaForce said. (LaForce later went on to join Serum, and worked for the company until his retirement in 2023.)
Most importantly, Serum was willing to join the project. As a 2003 paper by LaForce and his team notes, what was an opportunity cost for western manufacturers was an opportunity for the still growing Pune firm: a chance to gain a new skill set and to reach a new market, while receiving financial and technical help.
The Meningitis Vaccine Project eventually turned into a multi-continent partnership. The US FDA licensed its conjugation technology, while a Dutch private manufacturer licensed its polysaccharide manufacturing technology. Serum, by now an expert, made the tetanus toxoid, which they then conjugated with the polysaccharide, and manufactured the vaccine.
The development wasn’t a cakewalk. It took ten years, and many missteps, before MenAfriVac, (as the vaccine was eventually called) was prequalified by the WHO in 2010. But the vaccine that resulted was perfect for the meningitis belt: It cost just 40 cents per dose. Serum had also designed MenAfriVac to be heat stable, a feature no other meningococcal conjugate vaccine had. It was eventually purchased by UN agencies and GAVI, and led to Africa’s meningitis outbreaks declining within five years.
How did Serum achieve such low costs? Manufacturing at the scales required for African countries helped. But Serum also worked hard with the US FDA to increase the yields of its conjugation technology, bringing it up to 35 to 40%, LaForce told me. In contrast, the Sanofi meningitis vaccine used more inefficient conjugation technologies, yielding as little as 1 to 5%. The low efficiency didn’t matter to Sanofi, but it did make a difference to Serum, which couldn’t price its vaccine over 50 cents, said LaForce. Despite the huge impact such cost-cutting innovation has had on improving vaccine availability in poor countries, western manufacturers often use the phrase “me too” as a pejorative. “‘They say: You don't do enough. That's just me too stuff.’ Okay, fine, but the ‘me too’ stuff is the stuff that delivers the goods to hundreds of millions of people each year.”
More in house work, greater independence
Starting in 2008, Serum began two more product development partnerships with PATH, one funded by the Gates Foundation and another by the UK’s Foreign, Commonwealth & Development Office. Both upped the ante for the manufacturer: The goal was not only to make conjugate vaccines, but to make “multivalent” conjugate vaccines targeting multiple bacterial serotypes.
The first of these partnerships was to develop a conjugate jab against ten serotypes of Streptococcus pneumoniae, a respiratory bacterium that is the main cause of community acquired pneumonia (and sepsis in those with HIV). The second was aimed at improving MenAfriVac. The introduction of MenAfriVac led to a decline in serotype A outbreaks. As a result, new serotype outbreaks emerged. MenFive, the successor to MenAfriVac, would target four of these new serotypes, alongside the original serotype A.
Both projects presented obstacles orders of magnitude more challenging than MenAfriVac. “You had so many things that could to go wrong,” said Seattle based immunologist Mark Alderson, who was with PATH at the time and led the NGO’s collaboration with Serum on both the pneumococcal conjugate and MenFive vaccines.
In the case of the pneumococcal vaccine, there was an urgent need for a low cost alternative. Around the time Serum began working on it, there were only two WHO prequalified versions of the jab, by Pfizer and GSK. Pfizer’s pneumococcal conjugate vaccine, Prevnar, protected against 13 subtypes of S. pneumoniae, while GSK’s Synflorix protected against 10.
GAVI was buying these vaccines at high prices – $7 per dose. Other manufacturers like Sanofi and Merck had attempted to develop me too versions, but hadn’t succeeded yet.
Serum managed to pull off something even major developers were struggling with. The company had grown since its last PATH partnership and was now making more key R&D decisions on its own. And some of these decisions turned out to show remarkable foresight, like the development of a new, higher yield manufacturing process for toxoids. The older manufacturing process, which Serum used in the production of MenAfriVac, involved fermenting tetanus bacteria in large steel vessels and then isolating the toxoid. This time around, Serum had learned about a California based biotech firm, Pfenex Incorporated, which used a new recombinant technology that involved engineering a bacterium called Pseudomonas fluorescens to make the toxoid instead. This led to less raw material loss.
According to Alderson, few other vaccine developers had recognised the potential of Pfenex’s technology. This allowed Serum to license it when it was still affordable. Serum then fine tuned the technology and used it for both the pneumococcal vaccine and MenFive. The move proved prescient. The Pfenex technology eventually grew popular. Developers like Merck began using it too. Its licensing fee increased in step with its popularity, eventually rising much higher than what other LMIC manufacturers could afford. “I give Serum a lot of credit for what they did,” Alderson told me, “because they did it before anybody else.”
MenFive was prequalified in 2023, while Pneumosil was prequalified in 2019. The former was sold at $3 per dose to UNICEF, and the latter to GAVI at $2 a dose. At the time of its prequalification, Pneumosil’s price was 30% lower than the price that Pfizer and GSK were charging GAVI.
The Serum model
MenAfriVac, MenFive and Pneumosil are only three of Serum’s portfolio of over 25 vaccines today. But their development showcases the key strategies Serum has used historically to launch complex vaccines: making second line alternatives to existing vaccines, relying on in licensing and collaborations, defraying expenses with philanthropic funds, and investing in economies of scale.
While most Southern manufacturers use this mix of strategies, Serum is in a class of its own when it comes to large scale manufacturing. In 2007, Cyrus Poonawalla decided to increase Serum’s manufacturing capacity from 600 million doses to over 1 billion doses per annum, making it the largest manufacturer in the world. Manufacturing at this scale is not just about building a big factory: It also means knowing how to develop efficient processes that can lower the cost of manufacturing even further. According to Alderson, “This is where Serum got the lead over their competitors, including other Indian manufacturers. Some of them obviously have made good progress, but not to the same extent as Serum.”
Serum’s ability to work with large scales made global headlines during the COVID pandemic, when the world suddenly needed billions of vaccine doses at once. Serum increased its production capacity from 1.5 to 4 billion doses annually, using a combination of their own funds and support from the Gates foundation. In 2021, Serum became the largest manufacturer of a new COVID vaccine developed by Oxford University and licensed to British developer AstraZeneca. The plan was for AstraZeneca and others to supply to high-income countries, while Serum alone would supply to LMICs.
Serum was chosen because nobody else had the ability to work with the kind of scales, said Alexander Douglas, a pharmaceutical scientist at the Oxford University’s Jenner Vaccine Institute, who headed its manufacturing scale up team. Despite the expansion, however, things didn’t go as planned. Serum ended up missing its supply commitments to several LMICs, including African nations that were relying on it heavily. The incident led to a global reckoning about the African dependence on Indian manufacturers.
Domestic manufacturing or economies of scale?
In March 2021, India saw a large spike in COVID cases, as the more transmissible Delta variant began spreading in the country. In response, the Indian government banned vaccine exports. All production was diverted to local use.
By this time, Serum had already promised millions of doses of the Oxford/AstraZeneca vaccine to COVAX, a pooled procurement program for COVID vaccines launched by GAVI. COVAX participants included 47 African countries with little or no local manufacturing capacity.
The export ban meant that these countries were left with fewer vaccines than they had planned for. Serum ultimately did resume its exports in November 2021, supplying over 2 billion COVID vaccine doses around the world through the pandemic. But in face of the exploding global demand even this was insufficient; ultimately, African countries received only 3% of the global COVID vaccine supply.
These events led to African Union leaders forming the Partnership for African Vaccine Manufacturing (PAVM), which announced a bold ambition in 2021: to produce more than 60% of the vaccines they needed locally by the year 2040. In its roadmap, the PAVM says it will prioritize the production of 22 vaccines, including routine vaccines like malaria and measles, for which Serum is a major global supplier.
For some of these vaccines, the African manufacturing ambitions are limited to the tail end of the manufacturing pipeline — the so called “fill and finish” stage, in which the firm will receive the bulk vaccine from a supplier and then formulate it into the final product. This is the least technically challenging stage of vaccine production and a good entry point into vaccine manufacturing for inexperienced firms. For other vaccines, including malaria and measles, the PAVM wants even the bulk to be manufactured within the country. In both cases, the PAVM hopes, African companies will receive help in the form of technology transfers from the leading global manufacturers.
The plan has several critics — among them, Serum. In a 2024 interview, the company’s current CEO, Adar Poonawalla, son of Cyrus, called the growing movement for domestic manufacturing “misguided.” His argument: Low cost manufacturing needs economies of scale, and African firms are unlikely to achieve it quickly, while Serum is far ahead of the game. As of today, the company has a tech transfer agreement with the South African manufacturer Aspen Healthcare, for the fill and finish phase of four vaccines, but none for bulk vaccine production. Adar has also spoken in favour of the WHO Pandemic Accord, adopted in May 2025, which may prevent the kind of shortages triggered by the Indian export ban during the COVID pandemic. As part of the accord, member countries must commit to donating 10 to 20% of their pandemic vaccine production to WHO.
Serum’s stance on African manufacturing isn’t surprising: There’s little incentive for the company to support bulk production in Africa. The tech transfer for bulk production is a complicated process, Alderson told me, and the move would also create competition for Serum’s own products. What’s more, the Pune manufacturer also has 2.5 billion doses of spare capacity today — extra capacity it built during the COVID pandemic, which has remained unused since.
Perhaps this is why Adar has been lobbying for an alternative strategy: He wants to reserve the 2.5 billion doses of spare capacity for future pandemics and outbreaks. When an outbreak creates increased demand for a vaccine, Serum can repurpose its facilities to supply whatever is needed. But because maintaining the spare capacity between outbreaks is expensive, this plan would require countries to pay in advance to reserve it, a kind of “premium” for “insurance” against pandemics.
It's unclear if African countries will buy Serum’s pitch rather than focusing on building their own capacity. But even if they don’t, African domestic manufacturing is unlikely to pose a challenge to Serum or Indian manufacturers anytime soon: Today, the continent’s manufacturers meet only 1% of their local demand and make only one WHO prequalified vaccine, while Indian manufacturers make around three dozen prequalified vaccines. For African manufacturers to compete with Indian quality and scale might take up to three decades, the time it took India to get from one prequalified vaccine to where it is today.
This situation makes some public health experts wonder if the entry of developing country firms into vaccine manufacturing has really lived up to its original promise. Among them is Nina Schwalbe, who heads Spark Street Advisors, a New York based firm that consults for GAVI, the Gates Foundation and other health NGOs. Schwalbe told me that in the public health community, there was a “false expectation” that with time, vaccine manufacturing in developing countries would result in widespread competition which would drive down vaccine prices, as has already played out in the generic drug industry.
But second generation vaccines are harder to manufacture than generic drugs, and the barriers to entry are high. This is why, Schwalbe said, the vaccine market continues to be an oligopoly even today, with a few vaccine manufacturers dominating production. Schwalbe and several other public health experts also don’t buy Serum’s argument that large capacities concentrated with one manufacturer, and reservable by other countries, will ensure global supply security. No country can estimate how much vaccine it needs in advance, and Serum will still get to decide pricing, a less than ideal situation for African countries, points out Mohga Kamal-Yanni, a health policy advisor to the NGOs UNITAID and People’s Medicines Alliance.
Should Serum develop a first in class vaccine?
Despite the large strides Serum has made since its start, it has never developed a first in class vaccine. Doing so might help it enter the highly profitable US market, where it currently has little presence. But the company is already very profitable — its operating margins have been over 50% for years. Developing a first in class product would require making much steeper investments in R&D than the company has made in the past — investments which might not pay off.
Some argue that developing new vaccines for LMIC diseases is an imperative for the Indian industry, if not Serum alone. Soham Sankaran, the founder of a Hyderabad based startup called PopVax, which is attempting to develop a broadly protective COVID mRNA vaccine , says Indian vaccine manufacturers have, by and large, shied away from taking big bets when it comes to vaccine R&D. This has resulted in a situation where most research into first in class vaccines, even for diseases of great relevance to LMICs, continues to be the domain of western manufacturers and public health agencies.
Western manufacturers tend to drag their feet with such research, given the poor returns they anticipate from LMIC markets. British company GSK nearly gave up its malaria vaccine and tuberculosis vaccine programs until the Gates Foundation stepped in to support development. Meanwhile, India has no advanced tuberculosis vaccine candidate, even though the country has the world's largest burden of TB, says Sankaran. Given the R&D talent that already exists there, “India is one of the best places, if not, the best place to actually develop these kinds of novel vaccines,” Sankaran argues.
It’s hard to tell if Serum will throw its hat into the novel vaccine ring. Funding such a vaccine, without hurting the company’s profitability, and without raising the prices of the vaccines it currently sells, may require the company to raise money from the stock market. But the Poonawallas have historically balked at going public. More recently, Adar has argued that being a private limited company allows Serum to make affordable vaccines, because shareholders would demand higher profits.
Today, this bet is more urgent than ever. As the U.S. government considers slashing funding for public health agencies such as the National Institutes of Health (which has historically conducted much early stage research into vaccines for LMIC diseases), it’s less clear how much novel vaccine research for such diseases will happen in the US — making it even more important for countries like India to pick up the slack.
If Serum does eventually develop first in class vaccines, it will become the rare company that combines the strengths of both the global north manufacturers and the global south ones: a company that makes both low priced me too vaccines and global firsts. It’s not impossible, but it will likely take a lot of work.