Last May, Kim Kardashian debuted as Beyond Meat’s chief taste consultant. In a commercial posted to Instagram, Kim takes a selfie with a taco, inhales deeply over a breakfast sausage link, and swoons while chewing an apparent mouthful of Beyond Burger — except, as many fans noticed, the burger half in her hands remains pristinely cut, evidently untasted. In fact, across the thirty-second clip, Kim never actually bites into anything. For this, she got dragged in the comments. The media pounced too: “Kim Kardashian Is Being Roasted for Her Beyond Meat Advert,” ran the BuzzFeed headline.
But not all of the near 20,000 comments were on Kim’s eating habits. In many, the skepticism centered on the rise — and the healthfulness — of plant-based meats. They implicated Beyond’s products (in no particular order) in indigestion, cellulite, and cancer. Fans implored other fans to “just read the ingredients,” that Beyond Meat is, among other things, “full of chemicals” (“really bad chemicals,” “a chemical shitstorm”), “unnatural,” and “freaky.” The products are “engineered, specifically, to fool our senses into thinking they’re whole foods,” when in reality they’re full of “toxic fats” and “high carbs” and lacking in “real nutrients.” Other commenters veered down the now well-worn algorithmic path to misinformation, the narrative running something like: Beyond Meat is a plot to take over American ranchland. It’s lab meat — “poison” — funded by Bill “Satan” Gates. And it’s now being promoted by Kim, who only play-acts vegan; in reality, we know she’s an omnivore because we know she eats small children.
Reactions to Kim Kardashian’s social media may not, of course, be representative enough for market research. But in hindsight, the eighth most popular person on Instagram getting ratioed over a 30-second clip augured what would become a less than encouraging year for the plant-based meat industry.
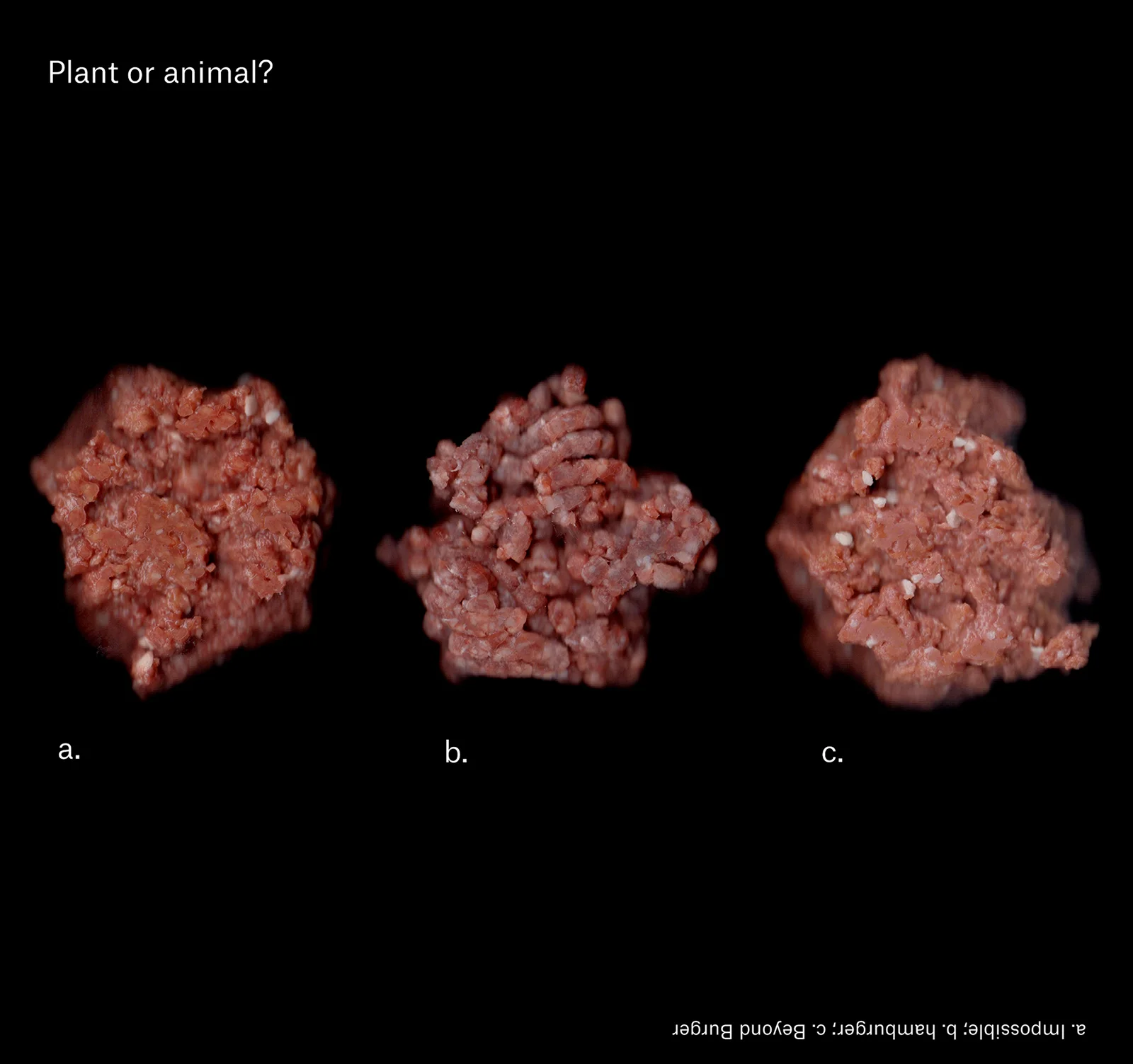
Before 2022, of course, the momentum had been building. The Impossible Burger debuted in 2016 to praise and optimism: Mark Bittman called it “impressive.” Ezra Klein called it “life-changing.” Restaurants in coastal cities served the then-limited supply on a first-come, first-served basis. McDonald’s, Burger King, and Dunkin’ debuted plant-based sandwiches. Both Impossible Foods and Beyond Meat struggled to meet consumer demand.
As retail availability expanded, sales increased steadily, around 10% per year. During the height of the pandemic, they exploded. In 2020, sales grew 45%, and the industry eclipsed the $1 billion mark for the first time.
Beyond Meat became a meme stock. Plant-based meats were heralded, at least in some corners of the internet, as a silver bullet, one of the best options to promote food system sustainability, combat global food insecurity, and minimize pandemic risk.
Sales held steady through 2021. For a moment, it felt like plant-based meat really was the future.
But 2022 was a bad year. Grocery sales dropped 14% by volume and restaurant orders were down nearly 10% from their 2019 peak. The press grew progressively worse, particularly for Beyond: McDonald’s ended their US trials of Beyond Meat’s McPlant (poor sales),
one factory was cited for “mold, listeria, and other food-safety issues,” and the company fired 19% of its employees.
(Impossible Foods announced in January 2023 that they too would be laying off 20% of their staff). Many outlets seemed eager to attack, the headlines oscillating between skepticism and eulogy: “Industry Possibly Suffering Perception Problem”; “Plant-Based Meat May Be All Hat, No Cattle”; “Fake Meat Was Supposed to Save the World. It Became Just Another Fad.”
What changed?
One answer is that the health halo around plant-based meats is dimming. In 2020, the Food Industry Association’s Power of Meat study found that 50% of consumers chose plant-based meat because they consider it healthier. Deloitte’s 2021 Future of Fresh survey put that number at 68%. But in 2022, health perceptions dropped: 15 percentage points in the Power of Meat survey, to 35%, and 8 percentage points in the Future of Fresh survey, to 60%.
There’s a Claude Lévi-Strauss quote that’s gone through a game of telephone as it’s been passed down through college syllabi. In its now garbled form, it’s become something of an axiom in food studies: good to eat, good to think.
The basic idea: Food must first be palatable to our values to be accepted; it must fit into our culture before it’s deemed fit for consumption. And consumers appear to be of many minds when it comes to plant-based meat.
Skeptics see a fabrication unlikely to escape the uncanny valley; foodies want a product that tastes better. Everyone wants a better price. But optimists look past the taste and see plant-based meats at scale: better for the planet, better for animals, and better for public health. Bruce Friedrich of the Good Food Institute, a nonprofit think tank dedicated to expanding the alternative protein market, includes two components in his theory of change: Plant-based meat won’t compete with animal agriculture until it costs the same or less and tastes as good or better. But there’s one “better” that’s missing from that formulation, the component a majority of consumers think about the most: better health.
Health Matters
People who eat fewer animal products do so because they think it’s better for them. In a 2019 Gallup poll, 23% of Americans reported reducing meat consumption in the prior year (5% were eating more). Of those eating less meat, 90% cited health reasons, and fully 70% named health a major concern — big gaps from concern over the environment, food safety, or animal welfare.
And global surveys by Euromonitor and Veylinx show similar patterns.
As the name suggests, plant-based meats have capitalized on the plant-based diet trend, and no company more so than Beyond Meat. The company’s IPO prospectus detailed the company’s “strong belief” that Beyond products can “help address concerns related to human health, climate change, resource conservation and animal welfare.” Ethan Brown, the company’s CEO, leans into health claims in particular. In 2021, he told The New York Times that “a No. 1 priority” is to “make sure people understand that our products are actually better for them than animal protein.”
But critics — and there are many — describe plant-based meats as ultra-processed foods (UPFs): highly energy-dense, “hyper-palatable” products. They slam the high sodium content, the ingredient list full of additives, or the heme iron found in Impossible.
And they are piggybacking off a growing body of evidence that links higher UPF consumption with pretty much everything bad: from all-cause mortality to decreased sperm motility. Michael Pollan’s advice — “Eat food. Not too much. Mostly plants.” — became a mantra of the food movement. By food, he meant “real” food: what your grandmother would recognize on the dinner table. Critics tap into this ethos: Meat is not a plant, but plant-based meat is not food. The Beyond Burger is, in Pollanian formulation, an edible foodlike substance, an intricate product of food science.
The health critique is being lobbed in some places you’d expect. Mark Bittman's blog Heated published a series of critiques of plant-based meat — “less like a salad, more like a Pringle.” Former Whole Foods CEO John Mackey has expressed reservations about the health impacts of plant-based meat, despite introducing Beyond Meat to the retail market. Academics worry the plant-based association obscures what could otherwise be a diet full of junk. But skepticism is also growing on the side of the aisle known to frequent Chick-fil-A and eat McDonald’s in the White House.
Since 2019, the Center for Consumer Freedom, a PR firm headed by Rick Berman,
has been leading a campaign against plant-based meats. Late in 2019, the organization placed full-page ads in The New York Times, The Wall Street Journal, and USA Today that raised health concerns over plant-based meats. The ads directed readers to CleanFoodFacts.com, where articles include “Bill Gates Wants You to Eat Ultra-Processed Goop,” “Quiz: Veggie Burger or Dog Food?” and “Titanium Dioxide in Meat: What Is It?” This January, the top “rising” topic searched in conjunction with plant-based meat on Google Trends was titanium dioxide. If Kim’s Instagram comments are indicative of anything, it’s that the ultra-processed means bad for you themes are catching on.
Berman and other opponents have exploited this opening. Taking a page from Steve Bannon’s playbook, the Center for Consumer Freedom’s strategy has been to flood the zone with shit — in this case, using evidence and language from nutrition science to run negative advertising in the form of full-page newspaper ads, a Super Bowl spot, even a campaign to force plant-based meats to include a cancer warning under California’s Proposition 65.
And that strategy seems to be working, because the zone’s been flooded with shit for a long time.
Definitive Evidence in Nutrition Science is Elusive
The nutrition debates
over plant-based meat typically center around one of two arguments: 1) Meat, especially red meat, is bad for you. Replacing beef with plant-based meats must therefore be better. This is the position of Beyond Meat and the Good Food Institute, among others. 2) Ultra-processed foods are bad for you, so plant-based meats are bad for you too. This is the where the Center for Consumer Freedom falls,
but it’s also the position of a constellation of actors that don’t necessarily want plant-based meat to fail. These include Carlos Monteiro, a professor at the University of São Paulo credited with spearheading research into food processing, and the International Panel of Experts on Sustainable Food Systems, whose recent report The Politics of Protein criticizes the framing of plant-based meats as a silver-bullet solution.
This debate will not be resolved in the short term. To understand why, it’s worth a short detour through the methods of nutrition science. We’ll look first at the evidence base around dietary patterns before diving into the specific research on plant-based meat. My goal is not to convince you that one position is right. It’s to show that because the literature is so messy, arguments from either side rely on spin as much as evidence.
The first issue is that nearly all studies purporting to show health consequences of eating (usually red) meat or health benefits of plant-based diets are observational. Observational studies are the backbone of nutrition science; they outnumber controlled trials in one estimate by more than 7-to-1. The basic idea is to follow people over a long time, record what they eat, and identify what foods or dietary patterns are associated with a range of health outcomes. Bigger studies and longer time frames equate to more statistical power and higher accuracy. But the limitations are considerable.
These studies have the same weakness as all observational research: showing that some health outcome is associated with a particular diet isn’t enough to prove that that diet caused the outcome. And in the world of nutrition, confounding is massive. People who eat healthier diets tend to look very different from those who don’t. Are improved health outcomes among vegetarians (if they are found, which is not always) due to the absence of meat or to a higher-quality diet? Might they be the result of demographic factors — higher income and education? Or is it something else entirely: higher health-consciousness, even religious belief? One meta-analysis of studies comparing heart disease between vegetarians and the general population found that beneficial effects for vegetarian diets was driven primarily by data from Seventh-Day Adventists; “the effect of vegetarian diet in other non-Adventist cohorts remains unproven.”
In addition to the challenges of observational research, nutrition science has a very difficult time accurately capturing dietary intake. How often did you eat bananas in the past year?
What about melons, strawberries, cooked greens, raw greens, stuffing, dressing, or dumplings? Vary the time scales in the questions, repeat for 140 foods, and you’ve completed a food frequency questionnaire. The most commonly used dietary assessment tools are bad. Like, open-secret, mostly unreliable bad. In 2013, Edward Archer, an obesity theorist, published an analysis of the data used in the CDC-sponsored National Health and Nutrition Examination Survey (NHANES) data set that showed that 60% of reported dietary intakes were physiologically implausible. Elsewhere, he’s called the data pseudoscientific and inadmissible in scientific research.
These challenges are part of why finding consensus in nutrition science is so difficult. Many observational studies indicate an association between meat consumption and negative health outcomes. Many do not. If you have priors, it’s extremely easy to confirm them by looking at isolated studies. One analysis of NHANES data demonstrated that high animal protein consumption led to increased mortality risk; another, using the same data, did not. Even meta-analyses are often unclear.
The strongest evidence of any risk is between processed meat and colorectal cancer. In 2015, the WHO took a strong position in classifying processed meat as carcinogenic.
But in 2019, a large analysis in the Annals of Internal Medicine looked at the same evidence combined with four new studies and concluded it was too weak to draw conclusions; the consortium of researchers ultimately recommended that adults continue their current meat consumption. Harvard scientists attempted to refute that. And then it emerged that the lead researcher behind the Annals of Internal Medicine studies and recommendation had in the past accepted funding from a trade group with ties to the meat industry. Nothing got resolved. This goes on ad nauseam.
The debate persists largely because, across a wide body of observational research relating to meat consumption and vegetarian dietary patterns, the evidence is inconsistent, the effect sizes are generally small, and the quality of evidence is very low. If you want to make a claim supporting meat consumption or vegetarianism, there are many studies — even many meta-analyses — you can choose from.
In experimental trials, we stand on somewhat firmer ground. And it’s here that we have direct evidence of some of the health impacts of plant-based meat.
Experimental studies have major advantages over observational research. Careful trial design can help tease out which foods actually impact our health, and shorter time scales permit researchers a more accurate look at what their subjects eat. Kevin Hall’s lab has pioneered the use of inpatient trials in a controlled environment where dietary intake and metabolism can be accurately monitored. Most notably, Hall demonstrated that a diet composed of ultra-processed foods results in increased energy intake and weight gain compared to unprocessed foods: If given no restrictions, people just eat more calories when they’re consuming UPFs. But most other experimental studies take place out in the real world.
Because these kinds of studies are costly and difficult to conduct over longer periods — very few people want to try experimental diets for months on end, let alone years — they can usually only track changes in short-term health outcomes or biomarkers like cholesterol or blood pressure. This is a big limitation, as we'll see. But a further challenge is that it’s extremely difficult to trust studies funded with industry support.
Over half of all industry-sponsored studies find favorable results, compared to 10% of studies without involvement. Sometimes the practice appears benign: For instance, when the California Strawberry Commission sponsors research on adult cognition. But it has also been insidious: Throughout the 1960s and ’70s, for instance, the sugar industry sponsored a research program that, according to a JAMA Internal Medicine article, “successfully cast doubt about the hazards of sucrose while promoting fat as the dietary culprit” in coronary heart disease.
Marion Nestle, professor emirata of nutrition, food studies, and public health at New York University, has written that industry funding has become so rampant that “health professionals and the public may lose confidence in basic dietary advice,” to say nothing about specific food products.
But public funding for nutrition trials is limited and industry interests are nearly limitless. Most trials sponsored by industry actors seem tailored to support specific talking points drummed up by marketing teams. That’s one way to read the most well-known trial on plant-based meat.
The SWAP-MEAT Trial
The most widely cited study on plant-based meats is the “Study With Appetizing Plantfood-Meat Eating Alternative Trial” — or, in the grand tradition of medical acronyms, SWAP-MEAT.
A brief summary
: SWAP-MEAT was a randomized crossover trial in which 36 participants ate two servings a day of either animal meat (ground beef, pork sausage, or chicken breast) or plant-based meat (Beyond products matched to the animal equivalents — Crumbles for ground beef, etc.). Each participant consumed the plant or animal diet for eight weeks, then switched to the other. Half began in the plant phase, half in the animal phase. The study’s primary outcome — the biomarker it measured — was fasting serum trimethylamine-N-oxide (TMAO, which we’ll get to shortly). Secondary outcomes were levels of cholesterol, triglycerides, glucose, insulin, blood pressure, and weight.
At the study’s end, TMAO was significantly lower during the plant phase than the animal phase. Participants in the plant phase also had significantly lower LDL (bad) cholesterol (on average 109.9 mg/dL compared to 120.7mg/dL) and weighed significantly less (on average 78.7 kg compared to 79.6 kg). The abstract concludes: “Among generally healthy adults, contrasting Plant with Animal intake, while keeping all other dietary components similar, the Plant products improved several cardiovascular disease risk factors, including TMAO; there were no adverse effects on risk factors from the Plant products.”
The Good Food Institute hailed SWAP-MEAT as “a critical milestone for alternative proteins.” Nestle, on her blog, was skeptical. She concluded that: “two servings a day of Beyond Meat is unlikely to be harmful. Whether substituting Beyond Meat for real meat is truly useful for health in the absence of other dietary changes remains to be confirmed, hopefully by independently funded research.”
The point, once again, is that your takeaway is likely to depend on your priors. And so in an effort to illustrate how much space there could be between positions, what follows is my most good faith argument between both positions.
Optimist: Bottom line: This study shows modest improvements in cardiometabolic biomarkers when plant-based meat is compared to the real thing. First, the differences in TMAO were huge! A 2017 systematic review of nearly 20,000 individuals showed that elevated concentrations of TMAO are associated with increased risk of both heart attacks and all-cause mortality. Several other studies, including a 2022 JAMA Network Open article, conclude the same. These are big studies in prestigious journals with large effect sizes. Now we have experimental evidence indicating the causal role played by meat, and plant-based products come out better.
Skeptic: The evidence on TMAO is unclear at best, meaningless at worst. TMAO is not a universally accepted biomarker of disease; no large health bodies condone its use as a diagnostic, and for good reasons. To nitpick one: TMAO is elevated in people with chronic kidney diseases, who we know have poor health outcomes — that association could explain some of those effects.
Even were that not the case, the use of TMAO as an indicator of disease is misleading. TMAO is produced when gut bacteria consume choline and carnitine, nutrients present in large quantities only in animal-sourced foods. Plant-based meats match animal meat on some nutrients, like iron, but they don’t have carnitine or choline. Saying that eating meat leads to higher TMAO relative to plants is something like saying that eating Skittles leads to insulin spikes relative to kale. Christopher Gardner, the study’s PI, admitted this in an interview when he described the TMAO result as a “foregone conclusion.”
Last point: Some fish are known to increase TMAO more than any other animal-sourced food — in one study, forty times more than red meat. Taking the logic of SWAP-MEAT at face value, we should also limit fish consumption — but fish is about the one thing most nutritionists agree is healthy.
O: Then let’s ignore TMAO, as, indeed, most write-ups of the trial have. On secondary outcomes, we stand on more solid ground. Body weights were lower during the plant phase of the trial (~2 pounds, on average). That’s a small but consistent difference — it wouldn’t have been significant otherwise. This finding provides evidence that counters the idea that plant-based meats will lead people to overeat because they’re “ultra-processed.” They might even lose weight!
S: But this result was only true for the group that received the plant intervention first. What’s more — and this is buried in the supplementary data — the plant-to-animal group gained weight on both diets. Meanwhile, the animal-to-plant group lost weight on both diets. Even if the main point of the study is to compare the plant and animal phases, it’s disingenuous not to discuss how the findings might generalize. If we care about relevance in the real world, shouldn’t we actually be looking at changes from baseline?
In addition (and forgive me for being a little conspiratorial here), the authors listed waist circumference as an outcome in their registration at ClinicalTrials.gov, but for some reason that isn’t included in the final report. I’m not necessarily calling foul — perhaps they concluded it wasn’t important — but I’m also not not calling foul. Two pounds may be statistically significant, but it’s hard to say it’s clinically meaningful, or likely to have an impact on health outcomes; it would be great to see another measure.
O: Fair. But the strongest evidence is that during the plant phase, participants’ LDL cholesterol was 10 mg/dL lower. Unlike two pounds of weight loss, this one is clinically meaningful. Meta-analyses have shown that a 10% decrease in LDL reduces all-cause mortality by something like 10%.
S: That’s true. But again, looking at baseline LDL levels suggests there’s noise within the signal. The plant-to-animal group came into the trial with mean LDL levels of 130. These dropped to 112 in the plant phase (a big drop!) before they rose to 122 in the animal phase. But even during the animal phase, the group's LDL levels were still lower than baseline. This is confusing because, before starting the trial, they were eating one serving of meat per day on average, compared to two during the trial. Somehow, even though they were eating more meat during the trial, their cholesterol was lower than before they enrolled.
The animal-to-plant group, meanwhile, began the trial at 113 on average, rising only 4 points to 117 during the animal phase before falling to 106 in the plant phase. The plant phase showed better LDL cholesterol overall, but the dose-response is inconsistent enough to make me wonder what would happen in a bigger trial.
That said, I do think it’s clear that LDL cholesterol was lower in the plant phase, but another question is: What about the fact that there were no differences in triglycerides or blood pressure? Or Insulin-like Growth Factor 1, which the authors hypothesized would change in their trial registration?
O: Plant-based meats have higher sodium, so the fact that the study found no meaningful differences in blood pressure is probably more in their favor. And macronutrients were fairly well matched in overall diets, so it’s not surprising that there weren’t larger differences in triglycerides.
S: I’m just not sure that’s conclusive enough to say that plant-based meat “improved several cardiovascular disease risk factors.” Regardless, a final point: Even if you think the findings are valid, they’re still an incomplete picture. In another study (which is similarly narrow, I’ll admit!), Itkonen et al. compared the impacts of varying ratios of animal to plant protein on bone health. After 12 weeks, participants in the plant-based diet had significantly higher markers of bone resorption and formation — risk factors for bone disease. We need so much more research!
The SWAP-MEAT study was specifically designed to make Beyond Meats look good, and it did so by choosing very specific biomarkers, only three of which showed changes, and even then the dose-response relationships were unclear. It was conducted by Christopher Gardner, who is vegan (no offense, Chris). And it was paid for through an unrestricted research gift from Beyond Meat to Stanford University. How do you tease out bias here?
O: The lack of restrictions on the research gift means Beyond had no involvement in any aspect of the study. And Gardner is a respected scientist with a track record of publishing null results. He wrote to Marion Nestle to tell her the study was coming. He’s well aware he runs the risk of being called a vegan shill. The point of this study was to answer questions specifically about plant-based meat compared to conventional meat. At worst, this study proves that, over a short period of time, eating plant-based meat is not bad for you. At best, it’s an indication that plant-based meats might be better.
The Limits of Reductionism
So, it’s hard to say that plant-based meats are healthier than animals. What of the argument that, as ultra-processed foods, they might actually be worse?
Over the past decade, the number of studies looking at food processing has exploded. It’s somewhat strange this didn’t start earlier — presumably our grandmas have been telling us all along that chips and Twinkies are bad for us — but the reason is that until 2010, we didn’t have a good way of thinking about degrees of processing. In that year, Carlos Monteiro first published the NOVA classification system for food processing, which now defines four processing categories
: unprocessed and minimally processed foods; processed culinary ingredients; processed foods; and ultra-processed foods. Unlike minimally processed and processed foods, UPFs are not modified whole foods; they are, under NOVA, “industrial formulations made mostly or entirely with substances extracted from foods, often chemically modified, and from additives, with little if any whole food added.” Most plant-based meats, including Impossible and Beyond, fall into this category.
Part of the reason we didn’t have good ways of thinking about food processing is that nutrition science had traditionally favored what’s usually called the reductionist approach — trying to understand how single compounds impact human physiology. This enabled massive strides in identifying and addressing micronutrient deficiencies, but it has more limited application to diet-related chronic disease. Beriberi is a thiamine deficiency, straightforwardly treated with a B1 supplement. The causes of coronary heart disease are multifactorial: stress, physical activity, air quality, smoking, diet, and potentially many more. They are difficult to tease out from one another, and it remains quite unclear how dietary substitutions impact the disease’s course. A Google Scholar search of “saturated fat” returns over 1.3 million articles, the top 10 of which are not in agreement. On a daily basis, this stuff leads to Twitter fights among grown adults.
The reductionist approach helped to transform the food landscape by incentivizing product reformulation. The canonical example is margarine, promoted as an alternative to saturated-fat-rich butter, the media’s favorite flip-flopping nutrition finding. After a series of articles showed small or neutral effects of butter on health outcomes, Time Magazine proudly proclaimed, “Eat Butter.” Those weary of the debate may prefer how Joan Dye Gussow, former chair of the nutrition education Program at Teachers College, put it: “I prefer butter to margarine, because I trust cows more than chemists.”
What’s glaringly absent within the reductionist paradigm — indeed, within much of nutrition science — is theory. Without it, much of nutrition science comes to resemble a frequentist fishing expedition amid a vast sea of data. This was memorably demonstrated in a 2013 article, “Is Everything We Eat Associated with Cancer?” Selecting 50 ingredients at random from a cookbook, including beef, lobster, corn, cinnamon, and rum, Jonathan Schoenfeld and John Ioannidis found that 80% had articles reporting on their cancer risk. Of 264 identified studies across the 50 ingredients, nearly three-quarters — 72% — showed statistically significant associations, including 103 of which showed increased risks for cancer. Theory demands causal mechanisms, but the status quo of nutrition science is to rely on previously reported associations.
The reductionist lens has seeped into the popular comparisons between beef and plant-based meat. In a piece in Wired, Hannah Ritchie argues that the backlash against processing unfairly characterizes plant-based meats. She compares the nutrition profile of grass-fed beef and plant-based meats, concluding, based on macronutrient profiles, that plant-based meats are “probably a bit better for our health than their meat equivalents.” But that analysis only incorporates protein, fat, saturated fat, and sodium. The Good Food Institute does a similar, selective comparison, which additionally includes cholesterol and fiber. But these products should not be viewed as nutritionally interchangeable even where nutrition panels appear similar. An analysis of plant-based meat and grass-fed beef showed substantial differences in nutrients (including some important ones) between meat and plant-based meat, despite the nutrition panels on packaging showing comparable nutrient profiles.
Moreover, the nutritional content of a food is not a perfect indicator of its ultimate fate in the human body, or of its health benefits. An analysis of 44 different meat substitutes available for purchase in Sweden found that while they contained similar amounts of iron to animal meat, this iron was in a form that’s much harder for our bodies to absorb. Phytate, present in many plant products, inhibits absorption of many nutrients, including iron. Generally, diets in high-income countries are sufficient in most nutrients for this not to matter, but where major micronutrient deficiencies remain common, phytate-to-nutrient ratios remain a concern.
Nutrient reductionism only tells us about specific nutrients in specific populations. That’s good for marketing claims, but it cuts both ways. It’s surprising that Big Beef hasn’t yet conducted a controlled trial of beef vs. plant-based meat in women with anemia, or even in children with stunting. But that may be because they don’t yet see a sufficient threat from the plant-based meat industry.
The SWAP-MEAT trial, to its credit, avoids nutrient reductionism. Others don’t. Good Food Institute’s Plant-Based Meat and Your Health: The Facts
favorably compares the Impossible Whopper to a conventional Whopper: “less total fat,” “more complex carbohydrates,” and “fewer calories.” Let’s ignore the fact that the differences in nutrients are quite small and focus on the larger health concern, which is that the Impossible Whopper from Burger King is an Impossible Whopper from Burger King. The same document, in a section that explains the “truth about processed food,” equates ruminant digestion to industrial food processing
while suggesting that foods like yogurt and olive oil are as highly processed as a plant-based burger.
The Center for Consumer Freedom may not be honest, but they are not alone in flooding the zone with shit.
A Giant Bag of Salt
Eliminating or reducing meat consumption asks 90% of people on the planet to change an integral aspect of their lives. Plant-based meats are supposed to make that change easier. Animal welfare and environmental advocates are probably the strongest proponents of these products. But health — not environment, not welfare — remains the strongest motivating force behind the plant-based buzz. In the process of attempting to convince consumers their products are healthier, corporations — Beyond, in particular — have adopted the same tactics as other large food industry players. This became most clear in November, when Beyond Meat announced to investors a partnership with the American Cancer Society to help “build the foundation of plant-based meat and diet data collection.” This is a big longitudinal study, but data on industry-funded research consistently shows a bias toward favorable results. Perhaps a market can decide on the most likely outcome for that study. For a company with a mission to “positively affect the planet, the environment, the climate and even ourselves,” intellectual honesty and transparency are two ingredients that are still missing. Without them, plant-based meats may never become good to think.
This goes too for the Good Food Institute, whose health messaging toes the line between spin and misinformation. “No matter which way you slice it,” reads their website, “plant-based meat has significantly more nutritional benefits than conventional meat. Whether it’s introducing a new source of fiber to your diet or cutting down on cholesterol, plant-based products lead to better health outcomes.” This is misleading at best. At its worst, it’s plainly wrong: There is no definitive evidence that eating plant-based meat leads to better health outcomes. And there’s no definitive evidence that it doesn’t. We have only the SWAP-MEAT trial and its short-term biomarkers.
But it does matter which way you slice it: Plant-based meats do come with trade-offs. These include higher sodium,
lower calcium, lower vitamin D, lower-quality protein, and lower bioavailability of the nutrients that plant-based meats claim to match in conventional beef, including iron. Big Beef can and will play the reductionist game too. These trade-offs may not be likely to matter to the average consumer, but they add up in the margins. Higher intake of red meat, for instance, is associated with better iron status even in high-income populations, and substituting animal protein with plant protein is shown to lead to decreased bone health. Moreover, it’s not at all clear that villainizing beef on fat and cholesterol makes plant-based meat look better than poultry, the consumption of which is rising much faster than beef is falling. And let’s not forget that eliminating beef does not require substituting plant-based meats. This is not a zero-sum game.
Up to now, industry entities aligned against plant-based meat have been relatively quiet on the media front, seemingly content with the Center for Consumer Freedom’s ultra-processed campaign and some scattered studies showing some benefits for beef. But should industry players choose to enter the academic fray and run their own experimental studies, it shouldn’t be surprising if deep pockets and some cleverly designed trials demonstrate evidence in support of conventional meat over plant-based meats: anemia, child growth, and bone health are obvious areas to target. If plant-based meat companies want to retain any competitive edge in public perception, it will help to avoid being grouped with Big Food or Big Tobacco. That halo won’t last long if their approach to scientific research is the same.
But at the moment, the plant-based meat industry should be more worried about scoring own goals. In January, Bloomberg’s Deena Shanker published a piece that described plant-based meat as a flop. Impossible responded by taking out a full-page ad in The New York Times. It featured a screenshot of three anonymous Reddit comments reacting to Shanker’s article. “I suspect it’s coming from a news outlet paid money to write a article by people who make money from meat sales,” said one. “It’s Bloomberg so i would take it with a giant bag of salt,” replied another. It was a strange look to publicize, at a cost of something like $250,000, an unsubstantiated claim about Bloomberg. More so still given that Impossible criticized the article — in a letter on their website — for failing to report the facts. To say nothing of the fact that one of the main critiques of their product is that it contains, roughly, a giant bag of salt.
Nutrition science is messy and hard. Given how difficult it is to arrive at definitive conclusions, this fight is not likely to end soon. Over time, financial influence from both sides may give us more evidence, but one result may be to make the conclusions less clear. The zone is flooded with shit, and more is coming. But the campaign to replace conventional meat with plant-based products should not underestimate what, in the public’s eye, is a 2-million-year incumbency in the human diet. The backlash to plant-based meat intuits this.
But we don’t even need to go that far back. Faced with sloppy, conflicting, and at times disingenuous messaging about a product that still costs more and tastes worse, it seems only rational if consumers continue to fall back on a simple heuristic: What would your grandmother eat?